The Growing Anxiety Epidemic
Globally, anxiety disorders are the most prevalent mental health disorder, with over 284 million people affected each year. In the U.S. alone, 40 million adults experience anxiety every year. The onset of the COVID-19 public health emergency has further contributed to soaring anxiety rates.
Reflecting this unfortunate reality, a national poll conducted in July 2020 found that 36.1% of U.S. adults reported symptoms of anxiety disorder based on having a score of three or greater on the clinically validated Generalized Anxiety Disorder (GAD-2) scale. Empowering tools that can help manage anxiety in the moment each day are needed more than ever.
The Promise of Heart Rate Variability Biofeedback for Anxiety Disorders
Heart rate variability biofeedback can help mitigate the negative effects of anxiety by pumping the brakes on the nervous system’s fight or flight response. Heart rate variability is the measure of the variation in time between each heartbeat, which is controlled by our autonomic nervous system.
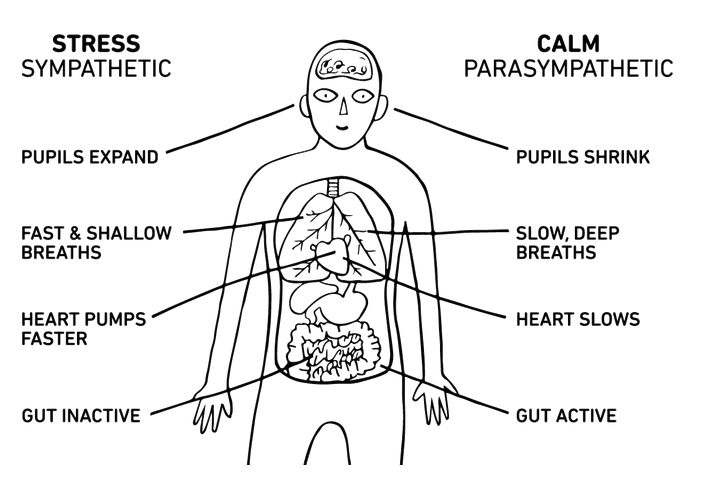
Our autonomic nervous system, divided into the parasympathetic “fight or flight” mode and sympathetic “rest and digest” mode, regulates automatic processes like breathing, heart rate, blood pressure, and digestion. Higher HRV indicates more optimal autonomic nervous system function, and can help reduce high blood pressure, depression, and anxiety. Biofeedback exercises, which sync respiratory and heart rate patterns, can increase heart rate variability.
The Warning Signal of Low Heart Rate Variability
Our autonomic nervous system constantly reacts to the information our brain processes throughout the day, whether that’s a stressful interaction with a family member or good news about a job promotion. Persistent negative instigators like poor sleep, stress, unhealthy diet, social isolation, and physical inactivity can disrupt the balance of the autonomic nervous system, causing the fight or flight response to shift into overdrive.
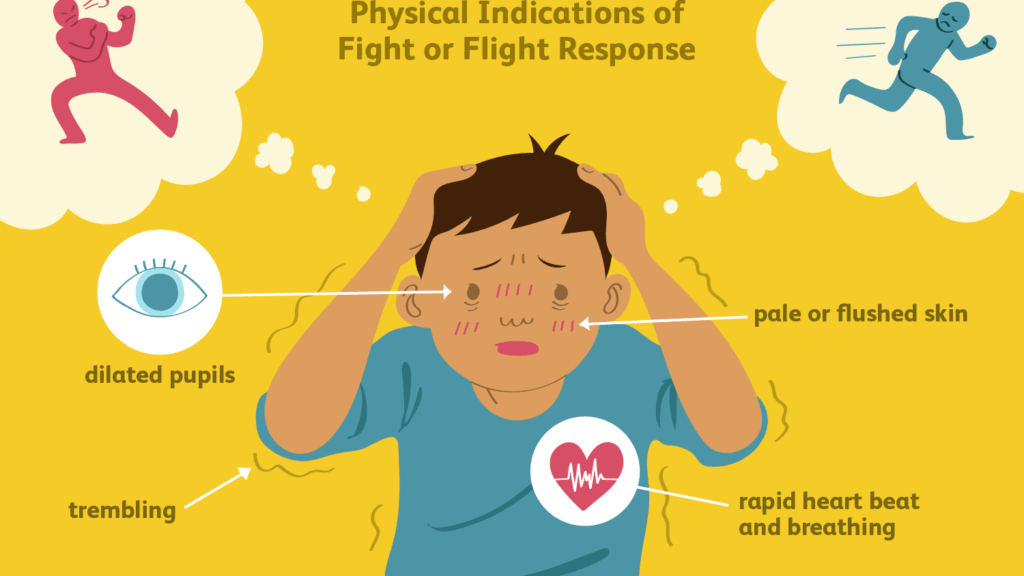
This over-activation of the fight or flight response is reflected in low heart rate variability. In this state, the autonomic nervous system is less able to efficiently switch gears, making it more difficult to bounce back from stressful triggers, and more likely that the body stays in “fight or flight” mode even when it’s not necessary. An overactive sympathetic nervous system is associated with anxiety disorders. As long as there is a perceived threat, the body’s stress response remains active, releasing cortisol to keep the body amped up, resulting in feelings of being on edge, worried, or anxious.
The Significance of the Vagus Nerve
To better understand why heart rate variability matters when it comes to anxiety, we must also understand the role of the vagus nerve. The vagus nerve is the longest nerve of the autonomic nervous system, originating from the brain stem and extending down through the neck, chest, and abdomen. It serves as a major mind-body highway that transmits information to and from the brain to the tissues and organs.
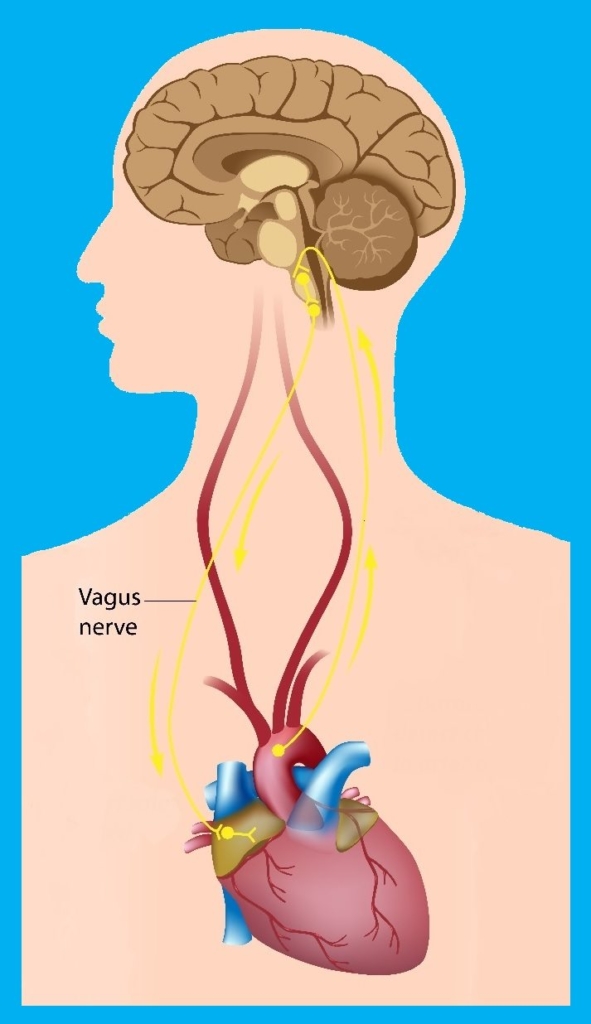
In the context of understanding anxiety, the vagus nerve represents the main component of the parasympathetic “rest and digest” mode of the nervous system, which oversees a vast array of crucial bodily functions, including control of mood.

The Vagus Nerve and Anxiety
The vagus nerve helps mobilize bodily responses depending on whether it senses safety or danger, even before such a cue enters conscious awareness. It instinctively scans the environment for signs of danger, as well as for safety.
The vagus nerve is the reason our breathing slows and our body relaxes when we’re chatting with a friend, and why our heart rate jumps and our stomach turns when we sense danger. It plays a central role in the autonomic nervous system, determining whether our body is in a state of calm or alarm, which then influences our emotional experience.

When we perceive we’re in a safe environment, vagal outflow increases, promoting regeneration, homeostatic functions, and social behavior. However, when the neural processes associated with the vagus nerve are impaired, we can become over-sensitive to perceived threats, even when there are none. Thus, we may have difficulty determining whether situations are safe or whether people are trustworthy, which contributes to the development of anxiety disorders.
Anxiety Disorders and Low Heart Rate Variability
Over the past few decades, research has highlighted the relationship between low heart rate variability and mental health, including anxiety disorders. A meta-analysis of 36 studies found anxiety disorders (e.g., PTSD, generalized anxiety disorder, panic disorder, social anxiety disorder) are associated with significant reductions in heart rate variability. The authors noted that medication use and medical and psychiatric co-morbidity did not impact the results.
A lens through which to interpret these findings is that anxiety, in all its forms, is ultimately indicative of reduced ability to inhibit cognitive (e.g., apprehension, vigilance, and worry), affective (e.g., panic), behavioral (e.g., avoidance), and physiological (e.g., increased heart rate) responses. This reduced capacity to regulate negative thoughts, emotions, and physiological responses leads to reduced vagal outflow, lowered HRV, and increased feelings of anxiety.

The significant reductions in heart rate variability found in the meta-analysis echoed previous theoretical models, indicating that the prefrontal cortex’s ability to regulate processes that contribute to the experience of anxiety are mediated by the vagus nerve, which is reflected in heart rate variability.
Activating the “Rest and Digest” Mode
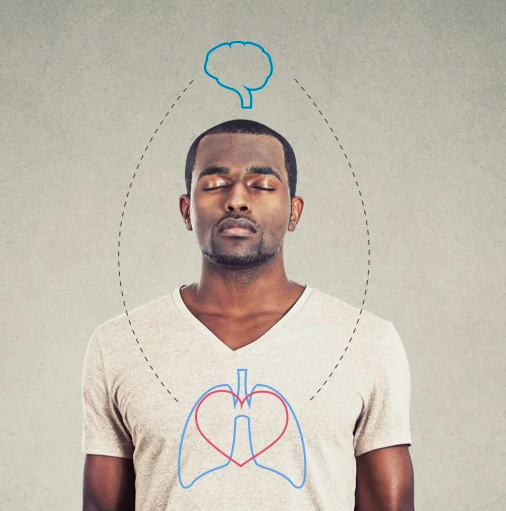
Fortunately, there is something that can be done to help restore reduced vagal outflow. When heart rate variability is low and the body is in fight or flight mode, it’s possible to restore relaxation and calm by directing vagal tone.
Vagal tone is measured by tracking heart rate alongside breathing rate. Our heart rate naturally accelerates when we breathe in, and decelerates as we breathe out. The bigger the difference in our heart rate when we inhale versus exhale, the higher the vagal tone. Higher vagal tone, reflected in higher heart rate variability, means the body is in an optimal state to recover more quickly from stressors.
Heart rate variability biofeedback helps restore vagal tone through slow and deep breathing exercises that sync heart rate with respiration. By doing so, heart rate variability biofeedback helps activate vagal pathways that counteract the flight-or-fight stress response. As a result, it lowers defenses, relaxes the body, slows heart rate, encourages feelings of centeredness and calm, and improves decision-making abilities.
Access an HRV Biofeedback Wearable Device with Clinical Grade Accuracy
In the past, the only way to access heart rate variability biofeedback was by going into a clinic. Now, this empowering exercise can be accessed anywhere throughout the day with a discreet wearable device. The Lief Smart Patch delivers automatic, personalized heart rate variability biofeedback practice throughout the day that proactively helps modulate the wearer’s autonomic nervous system.

Not only does Lief monitor heart rate variability in real time, it actively helps wearers increase their HRV whenever it starts to dip below the target threshold for that week. The Lief Smart Patch can be worn all day, enabling individuals to seamlessly incorporate HRV biofeedback into their daily lives no matter where they are, so acute feelings of anxiety can be reduced in real time as needed.





Leave a Reply
You must be logged in to post a comment.