An estimated 264 million people worldwide live with depression. In the U.S. alone, approximately 17.3 million adults have experienced at least one major depressive episode in the past year, according to the National Institute of Mental Health .
The link between heart health and mental health
Heart rate variability (HRV), the time interval between two successive heartbeats measured in milliseconds, is a noninvasive index of cardiac autonomic nervous system regulation. Depression and cardiovascular disease are interrelated, highlighting the importance of the relationship between heart rate variability (HRV) and mental health.
High HRV, where the autonomic nervous system is able to switch efficiently between its parasympathetic “rest and digest” and sympathetic “fight or flight” modes, indicates that the body is able to respond optimally to external triggers.
In contrast, low HRV indicates an autonomic imbalance, where the body is operating less efficiently between the two modes, and more likely to stay in fight or flight mode even when it’s not necessary or helpful.
Since the autonomic nervous system is responsible for regulating involuntary processes like heart rate, blood pressure, breathing, digestion, and emotional response, there has been growing interest in the relationship between low HRV and poor mental health outcomes.
Depression’s link to low HRV
Earlier meta-analyses indicate that HRV is lower in patients with major depression compared to those without across all age groups. A key distinction made in these findings was that lower HRV was not a specific feature of major depression, but rather a trans-diagnostic biomarker of mental illness indicating general dysregulation of the autonomic nervous system.
The consensus over the years has been that depression is associated with lower HRV. A 2018 study examining differences in HRV among 62 individuals with depression not taking antidepressants compared to 65 individuals without depression found reduced HRV in the depressed group. The authors interpreted these findings as reduced ability for the depressed group’s parasympathetic nervous system to regulate heart rate via vagal activity.
Echoing these findings, a meta-analysis of 21 studies including 2,250 patients and 1,982 controls found that all HRV measures were lower among individuals with major depression compared to those without. The authors concluded that such evidence provided strong support that lower HRV was a potential cardiovascular risk factor among individuals with major depression.

HRV as a casual factor of depression
However, these studies did not make clear whether depression affects heart rate variability or vice versa. In addition, previous research was limited in its ability to assess the relationship between HRV and depression over time. A more recent finding addressed these limitations using a longitudinal twin studies design.
Published in JAMA, a 146-pair longitudinal twin study found that low HRV is in fact causal to depression, not just associative. More specifically, this study found that lower HRV was independently associated with later increases in depressive symptoms. Unlike previous research suggesting that depressive symptoms corresponded to lower heart rate variability, the JAMA study found that such effects were not particularly robust, and were largely associated with antidepressant use.
These groundbreaking findings indicate that lower heart rate variability is more likely a risk factor for depression, rather than a consequence, and, at the very least, that the association between depression and HRV is bidirectional.
HRV biofeedback as a therapy to help treat depression
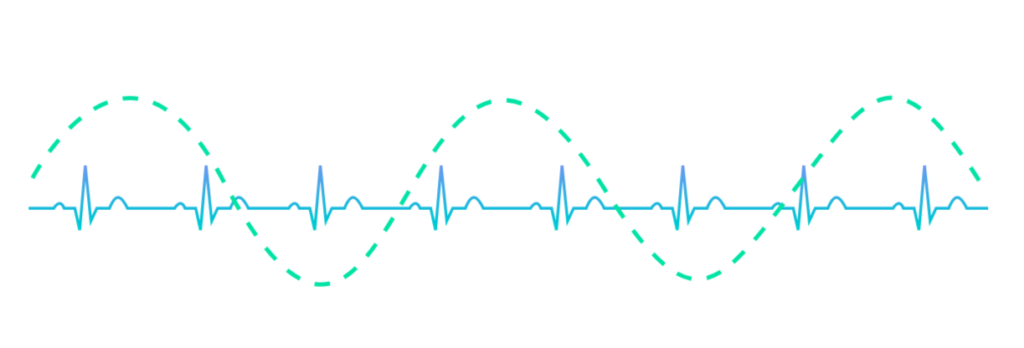
In addition to the link between HRV and depression, researchers have investigated the use of HRV biofeedback as a treatment modality for depression. Heart rate variability biofeedback training is a cardiorespiratory intervention that consists of feeding back beat by beat heart rate data during slow breathing maneuvers so that the individual tries to maximize respiratory sinus arrhythmia, create a sine-wave-like curve of peaks and valleys, and match respiratory sinus arrhythmia to heart rate patterns.
A randomized controlled study conducted over six weeks found that adding HRV biofeedback to psychotherapy not only increased HRV, but also improved the treatment of major depressive disorder. The study compared three groups: those who received HRV biofeedback in addition to psychotherapy, a psychotherapy only group, and a control group with no major depressive disorder.
The HRV biofeedback plus psychotherapy group demonstrated a larger increase in HRV and a larger decrease in depressive symptoms relative to the other two groups, which supports supplementing psychotherapy with HRV biofeedback when treating major depressive disorder.
Similarly, a case-controlled study conducted over six weeks, found that HRV biofeedback helped improve autonomic balance and symptoms of depression and insomnia in patients with major depressive disorder. The study looked at patients with major depressive disorder and insomnia compared to a control group. The treatment group received standard medical care and a weekly 60-minute HRV biofeedback protocol for six weeks, and the control group received medical care only.
The HRV biofeedback protocol included slow breathing at resonance frequency about 5.5 to 6 breaths per minute. The contents of the HRV biofeedback training included self-guided muscle relaxation, diaphragmatic breathing, paced breathing, pursed lip breathing, psycho-education of depression regulation, and a 10-minute daily homework.

Results of the 2019 case-controlled study demonstrated that patients with major depressive disorder co-morbid with insomnia had significantly decreased symptoms of depression and anxiety, and improved insomnia and pre-sleep arousal after six sessions of heart rate variability biofeedback training.
The promise of HRV biofeedback for depression
These studies examining the positive impact of HRV biofeedback training on major depressive disorder further support that HRV biofeedback potentially provides non-invasive, effective psychophysiological interventions for psychiatric disorders. A systematic review of 63 studies found that multi-modal biofeedback, such as electroencephalographic biofeedback combined with respiration biofeedback, appeared to most effectively alleviate symptoms, indicating that targeting more than one physiological modality for bio-regulation increases therapeutic efficacy.

A wearable smart patch for better mental health through HRV biofeedback training
Lief is the world’s first smart patch capable of delivering on-demand, personalized HRV biofeedback exercises throughout the day as needed. The Lief Smart Patch not only detects low HRV levels in real time, but helps wearers improve it using patented, haptic training exercises that can increase HRV in a few brief minutes using guided breathing exercises. Breath and heart rate are guided to be in sync to create respiratory sinus arrhythmia, the cyclic rise and fall of the heart rate in rhythm with breathing, activating the autonomic nervous system’s parasympathetic “rest and digest” mode.

As the evidence on the connection between low HRV and depression grows, awareness about tools that can help regulate HRV through empowering biofeedback exercises is more important than ever. Millions of individuals can benefit from this non-pharmaceutical stand alone or adjunct treatment option that helps manage stress at the physiological level.





Leave a Reply
You must be logged in to post a comment.